Nasopharyngeal Airway: 5 Critical Risks You Must Avoid When Using a Nasopharyngeal Tube
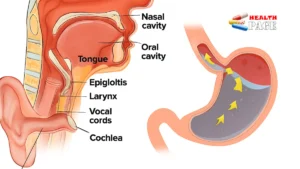
A nasopharyngeal airway is a soft, flexible tube that is inserted through the nostril and sits in the passage between the nose and the back of the throat. It is often called a nasopharyngeal tube or simply an “NPA.”
Its main purpose is simple: to help keep the airway open so air can move in and out more easily. It is most commonly used in situations such as:
- A person has reduced consciousness and their tongue might block the airway.
- There is a need for basic airway support while waiting for more advanced care.
- The mouth cannot be opened easily, or an oropharyngeal airway is not well tolerated.
The nasopharyngeal tube is designed to be less stimulating than some other airway devices, which can make it more comfortable for semi-conscious patients. However, that does not mean it is harmless or suitable for everyone.
It is important to remember: using a nasopharyngeal airway is not a casual first-aid step for untrained people. It is a clinical procedure that should be performed by healthcare professionals or properly trained responders, following local protocols and guidelines.
Why Understanding the Risks Is a Benefit to You and Your Patients
It may feel worrying to read about risks, but knowing them clearly is actually a major benefit. When you understand what can go wrong with a nasopharyngeal tube, you are far more likely to:
- Choose the right patients who will truly benefit from the device.
- Recognize early signs that something is not right and act quickly.
- Protect patients with hidden conditions such as nasal fractures or nasopharyngeal carcinoma.
- Use your skills with more confidence, instead of guessing in a crisis.
With that in mind, let’s walk through the five critical risks you must avoid, and how each one can become a benefit when you know what to look for and what to do.
Risk 1: Avoiding the Risk of Using the Wrong Size Nasopharyngeal Tube
Choosing the correct size is one of the most basic, yet most commonly overlooked, aspects of using a nasopharyngeal airway. A tube that is too short or too long can both cause serious problems.
What Can Go Wrong With the Wrong Size?
If the nasopharyngeal tube is too short:
- It may not reach far enough to keep the airway open.
- The tongue can still fall back and obstruct breathing.
- You may get a false sense of security, thinking the airway is protected when it is not.
If the nasopharyngeal tube is too long:
- It can go too far down the throat and cause gagging or vomiting.
- It may stimulate the larynx and trigger laryngospasm, making breathing suddenly worse.
- It can increase discomfort and the risk of trauma inside the airway.
How Correct Sizing Protects Your Patient
Correct sizing is a benefit because it allows the device to do its job without adding new dangers. When a properly sized nasopharyngeal airway is in place, you are more likely to see:
- Improved airflow without excessive stimulation of the throat.
- Better tolerance in semi-conscious patients, compared with some other airway devices.
- Greater overall stability of the airway while you monitor or provide further care.
In practice, this means taking an extra moment to choose the correct size rather than just reaching for whatever is closest. This small step can greatly reduce complications and improve outcomes.
Risk 2: Preventing Trauma, Bleeding, and Pain in the Nose and Throat
Because the nasopharyngeal airway is inserted through the nostril, it passes through delicate tissue that is easily injured. When insertion is rushed or rough, you increase the risk of trauma and bleeding.
What Can Go Wrong During Insertion?
Common issues include:
- Scraping the lining of the nose, leading to a nosebleed.
- Causing small tears that become painful and can become infected.
- Pushing against resistance instead of reassessing, which can damage tissue or the turbinates inside the nose.
In some patients, especially those on blood thinners or with clotting disorders, even a “minor” nosebleed can become a significant problem. Blood in the throat can increase the risk of aspiration, making breathing and airway protection much more difficult.
Why Gentle Technique Is a Real Benefit
By using a gentle, patient, and well-lubricated technique, you gain several benefits:
- Reduced pain and distress for the patient.
- Lower chance of bleeding that can complicate airway management.
- Better cooperation from semi-conscious or confused patients.
A small example: instead of forcing the nasopharyngeal tube through a tight nostril, choosing the other nostril or reassessing your approach can prevent an unnecessary injury. This is where skill and patience matter as much as knowledge.
Risk 3: Recognizing Contraindications, Including Nasal Injury and Nasopharyngeal Carcinoma
One of the biggest safety benefits of understanding the nasopharyngeal airway is knowing when not to use it. There are certain conditions where inserting a nasopharyngeal tube can be extremely dangerous.
Serious Contraindications to Watch For
Key situations where a nasopharyngeal airway may be contraindicated include:
- Suspected or known basal skull fracture (for example, after severe head trauma).
- Obvious severe facial or nasal fractures.
- Clear fluid (possibly cerebrospinal fluid) leaking from the nose after head trauma.
- Known tumors in the nasal passages or upper throat, including nasopharyngeal carcinoma.
- Significant obstruction in the nasal passage on examination.
In the case of nasopharyngeal carcinoma, the tissues in the back of the nasal cavity and upper throat are often fragile and may bleed easily. For someone with this type of cancer, forcing a tube through that area could cause significant bleeding, pain, and disruption of the tumor site.
How Avoiding These Situations Protects the Patient
When you pause and ask, “Is a nasopharyngeal airway safe in this specific patient?” you gain powerful benefits:
- You avoid rare but serious complications, such as a tube entering the cranial cavity in cases of basal skull fracture.
- You protect vulnerable tissue in conditions like nasopharyngeal carcinoma or recent nasal surgery.
- You are more likely to choose a safer alternative airway strategy when needed.
This is where clinical judgment becomes essential. The benefit of understanding these contraindications is that you can prevent harm while still providing effective airway support through other methods.
Risk 4: Reducing Infection Risk Through Good Hygiene and Handling
Any device that goes into the body can potentially introduce germs. A nasopharyngeal airway is no exception. Poor handling and hygiene increase the risk of infection, both for the patient and for healthcare workers.
How Infections Can Arise
Risks include:
- Using a nasopharyngeal tube that is not clean or has been improperly stored.
- Reusing single-use devices or sharing between patients, even briefly.
- Handling the tube with ungloved or contaminated hands, then inserting it.
These practices can lead to infections in the nose, throat, or lower respiratory tract. In vulnerable patients, such as those with weakened immune systems, even a small infection can become serious.
How Good Technique Becomes a Real Health Benefit
When a nasopharyngeal airway is used with careful attention to hygiene, you gain several advantages:
- Lower risk of introducing new infections to a patient who may already be critically ill.
- Reduced exposure of staff to respiratory secretions and potential pathogens.
- Stronger overall infection-control practices within your team or facility.
This does not require complex steps. It means consistently using clean, appropriate equipment, following your facility’s infection control policies, and handling the nasopharyngeal tube with the same respect you would give any other invasive device.
Risk 5: Avoiding Delays in Definitive Airway Management
A nasopharyngeal airway is a supportive device, not a final solution. One of the subtle risks is becoming too comfortable with it and delaying more definitive airway management when it is clearly needed.
How Over-Reliance Can Cause Harm
Potential problems include:
- Continuing to rely on the nasopharyngeal airway when the patient’s breathing is worsening.
- Focusing on the tube instead of recognizing signs of respiratory failure.
- Delaying interventions such as bag-mask ventilation, advanced airway placement, or urgent transfer to a higher level of care.
If someone is deteriorating despite a nasopharyngeal airway, they may need more support – not simply continued dependence on the tube.
How Clear Planning and Escalation Benefit Safety
The real benefit of understanding this risk is that you learn to see the nasopharyngeal tube as part of a bigger plan, not the whole plan. That means:
- Monitoring breathing closely after insertion: rate, effort, and oxygen levels if available.
- Being ready to escalate to more advanced airway measures when indicated.
- Communicating clearly within your team about what the next steps will be if the patient does not improve.
In other words, the nasopharyngeal airway should buy you time, not replace the need for timely, definitive care.
Quick Overview: Risks and How to Avoid Them
Use this simple table as a quick visual reminder of the main risks and the actions that help you avoid them.
| Risk | What Can Go Wrong | How to Reduce the Risk |
|---|---|---|
| Wrong size nasopharyngeal tube | Poor airway support, gagging, or laryngospasm | Select the correct length and diameter before insertion; reassess if it seems ineffective |
| Trauma and bleeding | Nosebleeds, pain, blood in the airway | Use lubrication, insert gently, never force against resistance, consider the other nostril |
| Contraindications ignored | Severe injury in skull fracture or tumor, worsening condition | Check for head or facial trauma, known tumors like nasopharyngeal carcinoma, or CSF leak before use |
| Infection risk | Nasal or respiratory infections in a vulnerable patient | Use clean, single-use devices as recommended; follow infection control and hand hygiene |
| Delay in definitive care | Respiratory failure while relying on the tube alone | Treat the nasopharyngeal airway as a temporary measure; escalate care promptly when needed |
Safe Use Checklist for Trained Providers and Responders
This checklist is not a substitute for formal training, but it can help you think through the safe use of a nasopharyngeal airway in a structured way.
Before Insertion
- Confirm your level of training and local protocol allows you to use a nasopharyngeal airway.
- Assess the patient for major contraindications: severe facial trauma, suspected skull fracture, known tumors in the nasopharyngeal area.
- Select the appropriate size of nasopharyngeal tube for the patient.
- Gather necessary equipment, including lubrication and personal protective equipment.
During Insertion
- Explain briefly to the patient if they are semi-conscious, to reduce fear and resistance.
- Insert gently along the natural curve of the nasal passage, without forcing.
- Stop if you meet firm resistance or if there is significant pain or bleeding.
After Insertion
- Check that breathing has improved: observe chest rise, listen for airflow, and monitor if equipment is available.
- Secure the nasopharyngeal airway so it does not move or fall out.
- Continue to monitor closely and be prepared to escalate to more advanced airway interventions if needed.
Remember, no checklist replaces hands-on training. If you are not a healthcare professional or trained responder, you should not attempt to insert a nasopharyngeal airway yourself. Instead, call for emergency help and focus on basic life support steps you are trained to perform.
Frequently Asked Questions About the Nasopharyngeal Airway
1. Is a nasopharyngeal airway safe for everyone?
No. While it is generally safe in many emergency situations when used by trained providers, it is not suitable for everyone. People with suspected skull fractures, severe facial trauma, certain nasal deformities, or conditions such as nasopharyngeal carcinoma may be at higher risk of serious complications. A careful assessment is essential before using a nasopharyngeal tube.
2. Can a nasopharyngeal airway be used in a fully conscious patient?
It is sometimes used in patients who are partially conscious if they cannot maintain their own airway and cannot tolerate an oropharyngeal airway. However, a fully awake person may find it uncomfortable and may resist or remove it. The decision to use it depends on the clinical situation, the patient’s condition, and local protocols.
3. How long can a nasopharyngeal airway stay in place?
It is usually meant as a short-term measure. In many situations, it is used for minutes to a few hours while more definitive care is arranged. Leaving a nasopharyngeal airway in for an extended period can increase the risk of irritation, pressure injury, or infection, so it should be regularly reassessed by healthcare providers.
4. What is the difference between a nasopharyngeal airway and an oropharyngeal airway?
A nasopharyngeal airway goes through the nose and follows the natural curve of the nasal passage to the back of the throat. An oropharyngeal airway goes through the mouth and sits over the tongue. The nasopharyngeal tube is often better tolerated by some semi-conscious patients, while the oropharyngeal airway is more commonly used in deeply unconscious patients who have no gag reflex. Both require training and careful patient selection.
5. Can I keep a nasopharyngeal airway at home for emergencies?
For most people, the answer is no. Because the device requires specific training to use safely and carries real risks if used incorrectly, it is not recommended as a home emergency tool for untrained individuals. Focusing on skills like recognizing emergencies early, calling emergency services, and learning basic life support (such as CPR) is usually more appropriate.
6. Does using a nasopharyngeal airway prevent the need for intubation?
Not necessarily. A nasopharyngeal airway helps keep the upper airway open and can support breathing in the short term, but it does not replace the need for intubation or other advanced airway procedures when those are indicated. In fact, it is often used as a bridge while the healthcare team prepares for more definitive airway management.
Key Takeaways: Using a Nasopharyngeal Airway With Confidence and Care
The nasopharyngeal airway is a valuable tool in emergency and clinical care. When used by trained professionals, it can make the difference between an obstructed airway and a stable, breathing patient. Yet that same device can cause harm if it is used without proper assessment, sizing, or technique.
To recap the most important points:
- Choosing the right size of nasopharyngeal tube helps ensure effective airway support without unnecessary irritation.
- Gentle, well-lubricated insertion protects delicate nasal tissues and reduces bleeding and pain.
- Recognizing contraindications, including significant facial trauma and conditions like nasopharyngeal carcinoma, prevents potentially severe complications.
- Good hygiene and infection-control practices reduce infection risk for both patients and staff.
- Seeing the nasopharyngeal airway as a temporary support, not a final solution, helps you avoid dangerous delays in definitive airway management.
If you are a healthcare provider or trained responder, take time to review your protocols, refresh your skills, and discuss these risks and benefits with your team. If you are a patient or caregiver, use this information as a starting point for conversations with your medical professionals, rather than trying to use a nasopharyngeal airway on your own.
With clear knowledge, respectful caution, and good training, the nasopharyngeal airway can remain what it is meant to be: a powerful, supportive tool that helps people breathe more safely when they need it most.