Understanding CHF ICD 10: Everything You Need to Know
Chronic Heart Failure (CHF ICD 10) affects millions of lives worldwide, creating significant challenges for patients and healthcare providers. This serious condition develops when your heart can’t pump blood effectively, impacting your body’s ability to receive the oxygen and nutrients it needs.
The impact of CHF on health can be severe:
- Reduced quality of life
- Limited physical activities
- Frequent hospital visits
- Increased risk of complications
Medical professionals use ICD-10 codes to document and track CHF cases accurately. These standardized codes serve as a universal language in healthcare, ensuring:
- Precise diagnosis documentation
- Appropriate treatment selection
- Accurate insurance claims processing
- Effective communication between healthcare providers
Think of ICD-10 codes as detailed maps guiding healthcare providers through the complex landscape of CHF diagnosis and treatment. Each code tells a specific story about the patient’s condition, helping doctors make informed decisions about care plans.
Understanding CHF and its associated ICD-10 codes is crucial for both healthcare providers and patients. This knowledge ensures proper diagnosis, treatment, and management of this chronic condition, leading to better health outcomes and improved patient care.
What is Chronic Heart Failure (CHF)?
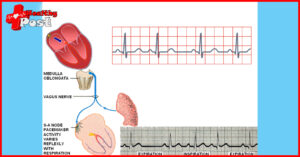
Chronic Heart Failure occurs when the heart muscle can’t pump blood effectively to meet the body’s needs. This condition develops gradually as the heart becomes weaker or stiffer over time. Unlike a sudden heart attack, CHF represents a progressive weakening of the heart’s ability to function properly.
Think of your heart as a pump in a complex plumbing system. When this pump starts failing, it affects the entire system – from blood flow to oxygen delivery throughout your body. The heart tries to compensate by:
- Enlarging to hold more blood
- Developing more muscle mass to pump stronger
- Pumping faster to increase blood output
- Narrowing blood vessels to maintain blood pressure
Types and Classifications of CHF
Left-Sided Heart Failure
The most common form affects the left ventricle – your heart’s main pumping chamber. When this occurs, you might experience:
- Shortness of breath, especially during activity
- Difficulty breathing while lying flat
- Wheezing or coughing
- Fatigue during daily activities
- Fluid buildup in the lungs
Right-Sided Heart Failure
This type often develops as a result of left-sided failure. The right ventricle struggles to pump blood to your lungs, leading to:
- Swelling in ankles and feet
- Enlarged liver
- Fluid retention in the abdomen
- Prominent neck veins
- General body swelling
Systolic vs Diastolic Heart Failure
Systolic Heart Failure
- Heart muscle becomes weak and enlarged
- Left ventricle can’t contract with enough force
- Blood isn’t pumped out strongly enough
- Common in younger patients
Diastolic Heart Failure
- Heart muscle becomes stiff
- Left ventricle can’t relax properly
- Heart can’t fill completely between beats
- More prevalent in older adults, women, and those with high blood pressure
The severity of CHF ranges from mild cases where daily activities are slightly limited to severe cases requiring constant medical attention. Medical professionals use a classification system called the New York Heart Association (NYHA) Functional Classification to determine severity:
- Class I: No limitation of physical activity.
The Role of ICD-10 in Diagnosing CHF
ICD-10 stands for International Classification of Diseases, 10th Revision – a standardized coding system healthcare providers use to document diagnoses and procedures. This universal medical language helps doctors, insurance companies, and healthcare facilities communicate effectively about patient conditions.
Healthcare providers rely on ICD-10 codes to:
- Track disease patterns and outbreaks
- Process insurance claims accurately
- Monitor patient outcomes
- Conduct medical research
- Make clinical decisions
Key ICD-10 Codes for Chronic Heart Failure
The ICD-10 system uses specific codes to identify different types and stages of heart failure. Here’s a breakdown of the most common CHF codes:
I50.9 – Heart Failure, Unspecified: This code indicates heart failure without specified type or cause. Doctors use it when initial symptoms suggest heart failure but further testing is needed.
I50.1 – Left Ventricular Failure: Used when the left ventricle can’t pump blood effectively to the body. Patients often experience shortness of breath, fatigue during physical activity, and difficulty breathing while lying flat.
I50.20-I50.23 – Systolic Heart Failure: These codes describe heart failure where the heart can’t contract normally:
- I50.20: Unspecified systolic failure
- I50.21: Acute systolic failure
- I50.22: Chronic systolic failure
- I50.23: Acute on chronic systolic failure
I50.30-I50.33 – Diastolic Heart Failure: Used when the heart can’t relax properly between beats:
- I50.30: Unspecified diastolic failure
- I50.31: Acute diastolic failure
- I50.32: Chronic diastolic failure
- I50.33: Acute on chronic diastolic failure
I50.40-I50.43 – Combined Systolic and Diastolic Failure: These codes indicate both contraction and relaxation problems:
- I50.40: Unspecified combined failure
- I50.41: Acute combined failure
- I50.42: Chronic combined failure
- I50.43: Acute on chronic combined failure
Recognizing Symptoms and Complications of CHF
Living with CHF requires careful attention to your body’s signals. Early recognition of symptoms can lead to timely medical intervention and better health outcomes.
Common Symptoms:
- Persistent shortness of breath during daily activities
- Unexplained fatigue and weakness
- Rapid or irregular heartbeat
- Swelling in ankles, feet, and legs
- Reduced ability to exercise
- Persistent coughing with white or pink-tinged mucus
- Difficulty breathing when lying down
- Need to urinate frequently at night
Serious Warning Signs:
- Sudden weight gain (2-3 pounds in a day)
- Chest pain or pressure
- Fainting or severe dizziness
- Confusion or impaired thinking
- Bluish discoloration of lips or fingertips
Potential Complications:
- Kidney damage or failure
- Heart valve problems
- Heart rhythm abnormalities
- Liver damage
- Sleep apnea
- Depression and anxiety
Untreated CHF can progress rapidly, leading to life-threatening situations. The heart’s reduced pumping capacity affects multiple organ systems, creating a cascade of health issues. The strain on your heart can cause it to enlarge, making it even harder to maintain proper blood flow throughout your body.
Regular monitoring of these symptoms helps track disease progression and enables healthcare providers to adjust treatment plans accordingly. Many patients find keeping a symptom diary helpful in identifying patterns and triggers.
Exploring Treatment Options for Chronic Heart Failure
Living with CHF requires a comprehensive treatment approach combining medication, lifestyle modifications, and regular medical supervision. Let’s explore these essential components of CHF management.
Medication Options
Several medications work together to improve heart function and reduce symptoms:
- ACE Inhibitors (like Lisinopril and Captopril) – relax blood vessels, lower blood pressure, and reduce strain on the heart.
- Beta Blockers (such as Metoprolol and Carvedilol) – slow heart rate, decrease blood pressure, and improve heart function.
- Diuretics (Water pills) – remove excess fluid, reduce swelling, and ease breathing difficulties.
- Aldosterone Antagonists – help the body maintain potassium, improve heart function, and increase survival rates.
Lifestyle Changes to Manage Chronic Heart Failure
Diet Modifications
A heart-healthy diet plays a crucial role in managing CHF:
- Limit sodium intake to 2,000mg daily
- Choose lean proteins
- Include whole grains
- Add plenty of fruits and vegetables
- Stay hydrated while following fluid restrictions
- Monitor daily weight to track fluid retention
Regular physical activity strengthens the heart and improves quality of life:
- Start with low-impact activities
- Aim for 30 minutes of exercise 5 days per week
- Include activities like:
- Walking
- Swimming
- Stationary cycling
- Light resistance training
Additional Lifestyle Adjustments
- Get adequate sleep (7-9 hours nightly)
- Quit smoking
- Limit alcohol consumption
- Manage stress through relaxation techniques
- Track daily symptoms in a journal
Medical Procedures
Some patients might need additional interventions:
- Coronary bypass surgery
- Heart valve repair
- Implantable devices
- Heart transplant in severe cases
Regular Monitoring
Track these vital measurements:
- Blood pressure readings
- Heart rate
- Weight changes
- Medication side effects
- Symptom changes
Taking Preventative Measures Against CHF
Preventing chronic heart failure starts with managing key health conditions that increase your risk. Here’s what you need to know about protecting your heart health:
Blood Pressure Management
- Monitor blood pressure regularly at home
- Take prescribed medications as directed
- Reduce sodium intake to under 2,300mg daily
- Practice stress-reduction techniques
Diabetes Control
- Check blood sugar levels as recommended
- Follow your prescribed diabetes management plan
- Schedule regular A1C tests
- Work with a diabetes educator for personalized guidance
Lifestyle Modifications
- Maintain a healthy weight through balanced nutrition
- Get 7-9 hours of quality sleep each night
- Quit smoking and avoid secondhand smoke
- Limit alcohol consumption to recommended levels
Regular Health Screenings
- Schedule yearly physical examinations
- Complete recommended cholesterol tests
- Discuss family history with your healthcare provider
- Report new symptoms promptly
These preventative measures work together to reduce your risk of developing CHF. Working closely with your healthcare team helps create an individualized prevention strategy based on your specific risk factors and medical history.
Conclusion
Understanding CHF and its ICD-10 codes empowers both healthcare providers and patients to navigate this complex condition. The detailed classification system helps track disease progression, determine appropriate treatments, and ensure accurate medical records.
Key Takeaways:
- Early recognition of symptoms leads to better outcomes
- Proper coding enables precise treatment plans
- Regular medical check-ups help monitor heart health
- Lifestyle changes play a crucial role in management
If you experience symptoms like:
- Persistent shortness of breath
- Unusual fatigue
- Swelling in legs or ankles
- Rapid heartbeat
Don’t hesitate to contact your healthcare provider. CHF symptoms can worsen without proper medical attention. A thorough evaluation using ICD-10 guidelines helps determine the specific type and stage of heart failure, leading to targeted treatment strategies.
Remember – your heart health matters. Medical professionals are equipped with the knowledge and tools to help you manage CHF effectively through proper diagnosis, treatment, and ongoing care.
FAQs (Frequently Asked Questions)
What is Chronic Heart Failure (CHF)?
Chronic Heart Failure (CHF) is a condition where the heart is unable to pump sufficiently to maintain blood flow to meet the body’s needs. It can be classified into left-sided and right-sided heart failure, as well as systolic and diastolic heart failure.
What are the key symptoms of CHF?
Common symptoms of CHF include shortness of breath, fatigue, and swelling in the legs or abdomen. If untreated, CHF can lead to serious complications such as kidney damage and liver problems.
How do ICD-10 codes relate to CHF?
ICD-10 codes are used in healthcare systems for diagnosing and documenting chronic conditions like CHF. They provide a standardized way to identify specific types of heart failure, allowing for accurate treatment and management.
What are some key ICD-10 codes associated with CHF?
Key ICD-10 codes for Chronic Heart Failure include I50.9 (Heart failure, unspecified), I50.1 (Left ventricular heart failure), and I50.20 (Systolic heart failure, unspecified). Each code helps in identifying the specific type and severity of heart failure.
What treatment options are available for managing CHF?
Treatment options for CHF typically include medications such as ACE inhibitors and beta-blockers, as well as lifestyle modifications like dietary changes and regular exercise to improve heart health.
How can one prevent Chronic Heart Failure?
Preventing Chronic Heart Failure involves managing underlying conditions such as diabetes and hypertension, maintaining a healthy lifestyle, and seeking medical advice if experiencing symptoms related to heart health.