Metformin: 7 Critical Facts About Side Effects, Weight Loss & Metformin 500 mg You Can’t Ignore
If you live with type 2 diabetes or insulin resistance, there’s a good chance you’ve heard of Metformin. It is one of the most prescribed medicines worldwide for blood sugar control. Many people also associate it with weight changes, stomach issues, and questions about long‑term safety.
You might be wondering:
- Are the metformin side effects really that common?
- Is metformin weight loss real or just a myth?
- What does metformin 500 mg mean for your dose and safety?
- How do you know if this drug is right for you?
This guide breaks down seven critical facts in clear, honest language. You’ll learn what the science says, what real people experience, and how to talk with your healthcare provider with confidence. 😊
Let’s walk through it step by step so you can feel informed, not overwhelmed.
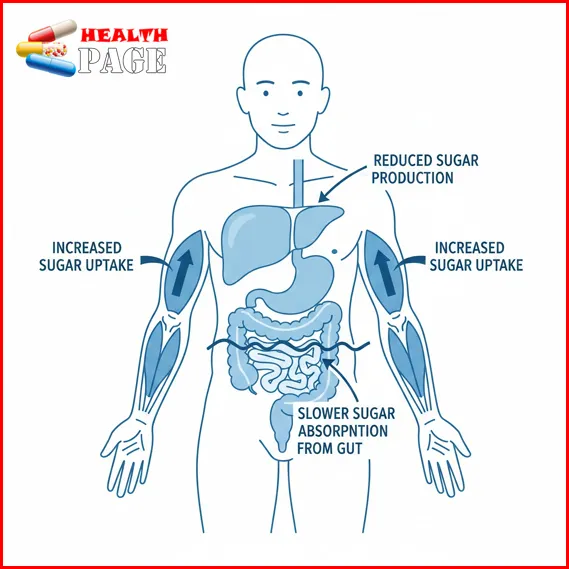
Fact 1: How Metformin Works Inside Your Body 🧬
Understanding how this medicine works can make everything else feel less scary.
Metformin belongs to a group of medicines called biguanides. It does not replace insulin. Instead, it helps your body use insulin more effectively.
It mainly works in three ways:
- It tells your liver to make less sugar.
- It helps your muscles absorb more sugar from your blood.
- It slightly slows how fast your body absorbs sugar from food.
Think of it as making your body less “stubborn” about insulin, rather than forcing your pancreas to make more.
Why this matters
Because it does not push your pancreas to pump extra insulin, it:
- Has a low risk of causing low blood sugar (hypoglycemia) when used alone.
- Is often used as the first medication for type 2 diabetes.
- Can be combined with many other diabetes medicines.
📝 Real‑life example:
Sam, 52, started this medicine after diet and exercise were not enough. Within three months, his A1C fell from 8.5% to 7.1%. He did not have low blood sugar, but he did notice some stomach discomfort at first.
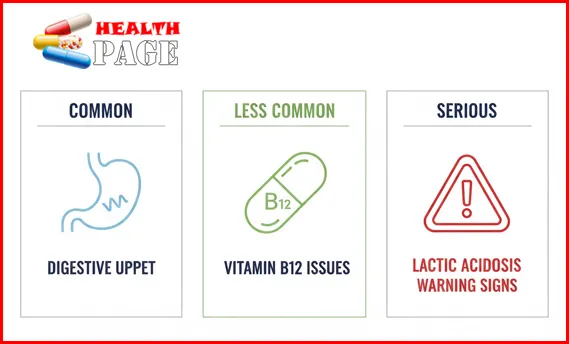
Fact 2: Common Metformin Side Effects Are Usually Digestive 🚽
The most talked‑about metformin side effects are stomach related. These can feel frustrating, especially when you are just starting.
Common side effects include:
- Nausea
- Stomach cramps or discomfort
- Bloating or gas
- Diarrhea
- A metallic taste in the mouth
- Reduced appetite
These usually appear:
- In the first days to weeks of treatment
- After a dose increase
- When taken without food
How long do these side effects usually last?
For many people, digestive symptoms:
- Improve within 1–2 weeks
- Can be reduced by taking the medicine with meals
- Become manageable with slower dose increases
Your body often needs time to adjust. It can help to think of this as a “getting used to it” phase.
Practical tips to ease common side effects
You can ask your healthcare provider about:
- Starting with a low dose and increasing slowly.
- Using an extended‑release version, which may be gentler on the stomach.
- Taking doses with a main meal, not on an empty stomach.
- Drinking enough water to reduce dehydration from diarrhea.
📝 Real‑life example:
Amina, 44, almost stopped her prescription because of diarrhea and nausea. Her doctor switched her to an extended‑release tablet and reduced the dose for two weeks. Her symptoms calmed down and her blood sugar improved over time.
Fact 3: Serious Side Effects of Metformin Are Rare but Important ⚠️
Most people do well on this medicine. Still, you should know the side effects of metformin that are less common but more serious.
1. Lactic acidosis (very rare but serious)
Lactic acidosis is a buildup of lactic acid in the body. It is extremely rare, but it is the most serious risk linked to this drug.
Seek urgent medical help if you notice:
- Unusual muscle pain or weakness
- Trouble breathing
- Extreme tiredness
- Slow or irregular heartbeat
- Feeling very cold, dizzy, or confused
- Stomach pain with nausea or vomiting
This risk is higher if you have:
- Severe kidney disease
- Serious liver disease
- Heavy alcohol use
- Certain conditions that reduce oxygen, like severe heart failure or a recent heart attack
This is why doctors check kidney function before and during treatment.
2. Vitamin B12 deficiency
Long‑term use may lower vitamin B12 levels in some people. This can cause:
- Numbness or tingling in hands or feet
- Weakness or fatigue
- Pale skin
- Memory or mood changes
Your doctor may test your B12 level, especially if you:
- Have anemia
- Are vegetarian or vegan
- Have long‑term digestive issues
3. Allergic reactions
Allergic reactions are uncommon, but can include:
- Rash or itching
- Swelling of lips, tongue, or face
- Trouble breathing
Seek emergency care if you notice signs of a severe reaction.
When to talk to your doctor urgently
Contact your healthcare provider right away if you notice:
- New or worsening shortness of breath
- Swelling in your legs, ankles, or feet
- Severe stomach pain, especially with vomiting
- Signs of low B12, such as new tingling or weakness
You deserve to feel safe and informed while taking any medication. 🚑
Fact 4: Metformin Weight Loss Is Real for Some, but Not Magic ⚖️
Many people are curious about metformin weight loss. Some even ask for this drug mainly to help with weight.
Here’s what research and experience show:
- Some people lose a small amount of weight (often 2–3 kg).
- Others mainly avoid gaining weight, compared with some other diabetes drugs.
- A few notice no change.
So, what is happening?
How this medicine may affect weight
Possible reasons for weight changes include:
- Reduced appetite in some people
- Mild nausea or changes in taste
- Better insulin sensitivity, which can affect hunger signals
However, it is not a fast or dramatic weight loss medication.
Who might notice more weight change?
People may see more impact when they:
- Combine the drug with healthy eating habits
- Increase physical activity
- Have insulin resistance or conditions like PCOS (polycystic ovary syndrome)
Even modest weight changes can improve blood sugar and overall health.
A realistic way to think about weight loss
It can help to see this medicine as a helper, not a hero. It may:
- Make it easier to avoid weight gain from other medicines.
- Support modest weight loss when paired with lifestyle changes.
- Improve health markers even if the scale barely moves.
📝 Real‑life example:
Carlos, 39, lost 3 kg over six months after starting treatment. He also began walking 30 minutes a day and reduced sugary drinks. The weight loss was slow, but his waist size and energy improved.
If weight is a big concern for you, ask your doctor about all options, not just one drug.
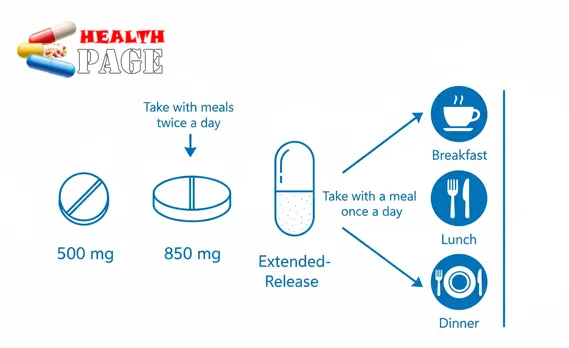
Fact 5: What Metformin 500 mg Really Means for Your Dose 💊
You will often see pills labeled metformin 500 mg. This simply means each tablet contains 500 milligrams of the active ingredient.
Most people do not stay on 500 mg per day. This is often a starting dose.
Typical dosing patterns
Always follow your own doctor’s instructions. Typical patterns might look like:
| Situation | Example Daily Dose | Notes |
|---|---|---|
| Starting dose | 500 mg once daily with evening meal | Helps your body adjust slowly |
| Early increase | 500 mg twice daily (breakfast, dinner) | Often after 1–2 weeks if tolerated |
| Usual effective dose range | 1,000–2,000 mg per day | Divided into 2–3 doses or extended‑release |
| Maximum recommended dose | About 2,000–2,550 mg per day | Depends on product and local guidelines |
Your doctor chooses the dose based on:
- Your blood sugar levels and A1C
- Your kidney function
- How well you tolerate the medicine
- Other medications you take
Immediate‑release vs extended‑release
You might see:
- Regular tablets (often taken 2–3 times daily)
- Extended‑release tablets (often once daily, sometimes twice)
Extended‑release tablets can reduce stomach upset for some people. They must be swallowed whole, not crushed or chewed.
Why dose changes happen
Do not be surprised if your dose changes over time. This may happen when:
- Your blood sugar improves or worsens.
- You start or stop other diabetes medications.
- Your kidney function changes.
Dose adjustments are not a failure. They are part of fine‑tuning your treatment so it fits your life and your body. 💙
Fact 6: Not Everyone Is a Good Candidate for This Medicine 🧪
While Metformin is widely used, it is not right for everyone. Your safety comes first.
Doctors are cautious or may avoid this medicine if you have:
- Severe kidney disease or rapidly worsening kidney function
- Serious liver disease
- Severe heart failure or unstable heart disease
- Frequent heavy alcohol use
- A history of lactic acidosis
You may also need to pause treatment in some situations, for example:
- Before certain imaging tests that use iodine contrast dye
- Before major surgery
- During severe dehydration, severe infection, or shock
Your clinician will guide you on when to stop and when to restart.
Important conversations to have with your healthcare provider
Before starting, tell your doctor if you:
- Have kidney or liver problems
- Have heart failure or lung disease
- Drink alcohol regularly
- Have a history of anemia or vitamin B12 deficiency
- Are pregnant, planning pregnancy, or breastfeeding
It can feel emotional to list all your health issues. Still, sharing this information helps your team protect you and choose the safest plan. 🫶
For clear patient‑friendly guidance, the NHS metformin patient information page is a helpful reference: NHS metformin patient information.
Fact 7: How to Make This Medication Work Best for You 🌱
Medicine is only one piece of your health puzzle. How you live with it day by day can shape both its benefits and its risks.
1. Take it consistently
Try to:
- Take your tablets at the same times each day.
- Link your dose to meals to help your stomach adjust.
- Use pill boxes, phone reminders, or alarms if you forget doses.
If you miss a dose:
- Take it when you remember, unless it is almost time for the next one.
- Do not double the dose to “catch up.”
2. Support your body with food and movement
This medicine works best when paired with:
- Balanced meals with vegetables, lean protein, and healthy fats
- Choosing whole grains more often than refined carbs
- Regular movement, even gentle walking or stretching
You do not need a perfect diet or intense gym routine. Small, steady steps add up. 🏃♀️
3. Monitor how you feel
Keep track of:
- Digestive changes
- Energy levels
- Weight trends
- Numbness, tingling, or mood changes
Share these with your healthcare provider at check‑ups. They can guide tests for vitamin B12, kidney function, and A1C.
4. Protect your mental and emotional health
Living with diabetes or insulin resistance is not just physical. It can affect mood, self‑esteem, and daily stress.
Consider:
- Talking openly with your clinician about fears or frustrations
- Joining a support group, online or in person
- Asking for a referral to a counselor if you feel overwhelmed
You deserve care that respects both your body and your feelings. 🧡

FAQs About This Common Diabetes Medication ❓
1. How long does it take to start working?
You may see changes in blood sugar within a few days, but the full effect can take:
- 2–4 weeks for daily readings to settle
- 3 months or more to see the impact on your A1C
Your doctor will usually check your blood tests after several weeks or months, not just a few days.
2. Can I drink alcohol while taking it?
Light to moderate drinking may be allowed for some people. Still, alcohol can:
- Raise the risk of lactic acidosis in high amounts
- Affect blood sugar control
- Add calories that affect weight
Always ask your clinician what is safe for you, especially if you drink regularly.
3. Is it safe to take long term?
For many people, this medicine is used for years. Long‑term safety is generally good when:
- Kidney and liver function are monitored
- Vitamin B12 is checked from time to time
- You report new or unusual symptoms promptly
Never stop long‑term medicines suddenly without medical advice.
4. Can I take it for prediabetes or PCOS?
Some doctors prescribe this medication for:
- Prediabetes, to help reduce progression to type 2 diabetes
- PCOS, to improve insulin resistance and menstrual cycles
Whether it is right for you depends on your health profile. Your doctor will weigh benefits against risks before deciding.
5. What if I cannot tolerate the side effects?
If metformin side effects feel unbearable, do not suffer in silence. Options may include:
- Lowering the dose
- Switching to extended‑release tablets
- Changing the timing with meals
- Considering a different diabetes medicine
Your comfort and quality of life matter just as much as your lab numbers.
6. Does everyone lose weight on it?
No. While metformin weight loss happens for some people, others notice very little change. Some simply avoid gaining weight. Focus on how you feel, your blood sugar, and your overall health, not just the scale.
Conclusion: Using Metformin Wisely and Confidently 🌟
Metformin has helped millions of people manage type 2 diabetes and insulin resistance. It can lower blood sugar, support modest weight changes, and fit well with other treatments. At the same time, side effects of metformin—especially stomach issues—can be challenging at first.
Key takeaways from these 7 facts:
- Digestive symptoms are common but often improve with time and dose changes.
- Serious risks like lactic acidosis are rare, but it is vital to know warning signs.
- Metformin 500 mg is usually a starting point, not a final dose.
- Metformin side effects and metformin weight loss vary widely from person to person.
- Regular check‑ups, honest conversations, and healthy daily habits make this medicine safer and more effective.
Your health journey is personal. Use this information to ask better questions, understand your options, and work as a partner with your healthcare team. With the right support, you can use this medication as one tool—among many—to move toward a healthier, more confident life. 💚


