Saddle Anesthesia: 7 Shocking Causes & Symptoms You Must Know
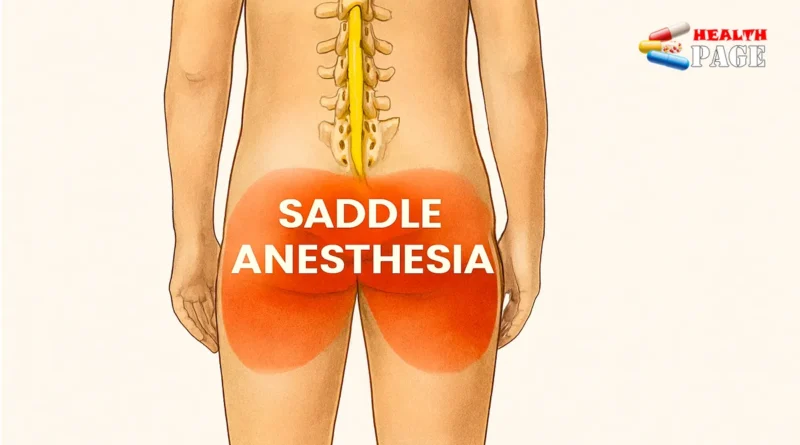
Feeling numbness or strange tingling in your groin, buttocks, or inner thighs can be terrifying. When doctors use the term saddle anesthesia, they mean numbness in the areas that would touch a saddle when you sit on a horse.
This is not a symptom to watch at home or “wait and see.” It often points to a serious problem affecting the lower spinal cord or the nerves leaving it. Some causes are medical emergencies that require treatment within hours.
In this guide, you will learn what saddle anesthesia is, which symptoms matter most, and the main conditions that cause it. You will also see how doctors test for it and when you should go straight to the emergency department.
The goal is to help you feel informed, not panicked. Understanding the risks helps you act quickly and protect your long‑term nerve function.
What Is Saddle Anesthesia?
People often ask, “What is saddle anesthesia in simple words?”
It means decreased sensation, complete numbness, or abnormal tingling in the “saddle” region:
- Around the anus
- The perineum (between genitals and anus)
- Inner thighs
- Buttocks
You might notice:
- Numbness to light touch, temperature, or pain
- A “cotton,” “asleep,” or “dead” feeling in those areas
- Burning, pins and needles, or electric shock sensations
This pattern suggests a problem in the lower spinal cord or the bundle of nerves at its base. That bundle is called the cauda equina, Latin for “horse’s tail.”
Because these nerves control bladder, bowel, and sexual function, changes in this area are a major red flag.
Common associated symptoms include:
- New difficulty starting urination
- Loss of bladder control or leaking without warning
- Trouble passing stool or losing control of bowel movements
- Weakness or heaviness in both legs
- Severe low back pain, often spreading down both legs
When doctors talk about saddle anesthesia symptoms, they are always thinking about possible nerve compression. Many causes require urgent imaging and sometimes immediate surgery.
How Doctors Check For Saddle Numbness
You may wonder about the “saddle anesthesia test” and what doctors actually do.
In clinic or the emergency department, the evaluation usually includes:
- A detailed history
- A focused neurological exam
- Imaging, often an MRI
Key parts of the physical and neurological exam:
- Testing light touch with a piece of cotton
- Checking pinprick sensation with a small, safe tool
- Asking whether cold metal feels cold in the saddle region
- Assessing anal tone with a gentle rectal exam
- Checking leg strength and reflexes
- Asking about bladder fullness, pain, and leakage
These checks help map exactly where numbness starts and ends. They also show whether the nerves controlling bladder and bowel already fail.
Imaging tests may include:
- MRI of the lumbar spine, usually the first choice
- CT scan if MRI is not available quickly
- Sometimes additional scans to look for tumors, infection, or fractures
Blood tests can help reveal infection, inflammation, or cancer markers.
The full picture tells your team which of the possible saddle anesthesia causes is most likely and how urgent treatment must be.

1. Cauda Equina Syndrome: The Most Urgent Cause
Cauda equina syndrome is the condition doctors fear most when they hear about saddle numbness. It happens when the nerve roots at the very bottom of the spinal canal become compressed or badly injured.
Common triggers include:
- A large lumbar disc herniation
- Spinal canal narrowing (lumbar spinal stenosis)
- Sudden bleeding in the spinal canal (epidural hematoma)
- Spinal tumors pressing on the nerve roots
- Severe trauma, such as a fall or car crash
Typical symptom cluster:
- New numbness in the saddle area
- Weakness in one or both legs
- Severe low back pain
- Shooting pain down the legs, often both
- Trouble starting to urinate, or complete retention
- Loss of bladder or bowel control
- Reduced sexual sensation
These saddle anesthesia symptoms often appear over hours, sometimes a day or two. The faster they appear, the more urgent the situation.
Real‑life example:
A 45‑year‑old person with long‑standing back pain suddenly loses feeling around the anus and cannot pass urine. In the emergency department, imaging shows a massive lumbar disc pressing on the cauda equina. Emergency surgery is done the same night to prevent permanent paralysis and incontinence.
Cauda equina syndrome is a neurosurgical emergency. Delays in diagnosis and treatment can lead to lifelong disability.
2. Conus Medullaris Syndrome: Damage At The End Of The Spinal Cord
The spinal cord ends around the level of the first or second lumbar vertebra. This tip is called the conus medullaris. Damage here can also cause numbness in the saddle area.
Causes include:
- Trauma to the lower spine
- Tumors growing in or around the spinal cord
- Spinal cord infarction (stroke of the spinal cord)
- Infections or inflammatory diseases attacking the cord
Conus medullaris syndrome can look similar to cauda equina syndrome, but there are differences:
- Symptoms often start suddenly
- Both legs may feel weak at the same time
- Reflexes in the legs may be brisk rather than absent
- Early loss of bladder and bowel control is common
Patients may describe:
- Numbness or burning pain between the legs
- Sudden changes in sexual function
- A “band” of numbness above the groin
Real‑life example:
Someone slips on ice and lands hard on their lower back. Within an hour, both legs feel weak, and they lose control of urination. Imaging reveals damage at the conus medullaris from a burst vertebral fracture.
This condition also requires urgent evaluation. Sometimes surgery can stabilize the spine and prevent further damage.
3. Spinal Trauma And Fractures
Major trauma is an obvious risk. Yet sometimes the injury seems minor at first. Later, numbness develops in the saddle region, which can surprise the person.
Traumatic events that may lead to this kind of numbness include:
- Car or motorcycle accidents
- Falls from height
- Direct blows to the lower back or pelvis
- Sports injuries, such as hard tackles or falls
Possible damage patterns:
- Vertebral fractures that narrow the spinal canal
- Dislocations that pinch nerve roots
- Bleeding into the spinal canal or around the cord
Symptoms to watch after trauma:
- New or worsening low back pain
- Leg weakness or heaviness
- Any change in sensation in the groin or anal area
- Difficulty urinating or changes in bowel patterns
Real‑life example:
A cyclist crashes and lands on their back. They walk away but feel worse over the next day. Numbness develops between the legs, and their urine stream weakens. Imaging later shows a small fracture fragment pushing into the canal. Prompt surgery prevents permanent damage.
Even if trauma seems minor, any new saddle area numbness is an emergency warning sign.
4. Spinal Tumors And Metastases
Not all causes arise suddenly. Some grow slowly over months. Spinal tumors can press on the lower cord or nerve roots, causing progressive numbness in the saddle region.
Types of tumors that may cause this include:
- Primary spinal cord tumors, such as ependymomas or astrocytomas
- Nerve sheath tumors near the cauda equina
- Metastatic cancers from breast, lung, prostate, or kidney
- Lymphoma or other hematologic cancers in the spine
Typical features:
- Gradually worsening low back pain
- Pain often worse at night or when lying down
- Weakness or clumsiness in the legs
- Numbness or tingling that starts in the feet and climbs upward
- Later, numbness in the perineum and around the anus
Real‑life example:
A 60‑year‑old with a history of breast cancer notices back pain and progressive leg symptoms for months. Then she loses feeling around the anus and has trouble controlling bowel movements. MRI reveals metastatic spread compressing the cauda equina.
Treatment options may include:
- Surgery to remove or reduce the tumor
- Radiation therapy to shrink it
- Chemotherapy or targeted therapies
- Steroids to reduce swelling around the cord
Even slow‑growing tumors can cause permanent disability if not detected early. Any new groin or anal numbness in someone with a history of cancer deserves rapid imaging.
5. Spinal Infections And Inflammatory Diseases
Infections and immune‑mediated inflammation can attack the spinal cord or its coverings. When this happens near the lower spine, numbness in the saddle region may develop.
Important infectious causes:
- Spinal epidural abscess, usually from bacteria
- Vertebral osteomyelitis (bone infection) spreading inward
- Tuberculosis of the spine (Pott’s disease)
Risk factors often include:
- Diabetes
- Intravenous drug use
- Recent spinal surgery or injections
- Immune suppression, such as from HIV or medications
Typical signs:
- Back pain that worsens over days or weeks
- Fever, chills, or night sweats
- General feeling of being unwell
- Local tenderness over the spine
- Later, leg weakness and saddle area numbness
Inflammatory causes can include:
- Transverse myelitis, inflammation of a segment of the spinal cord
- Multiple sclerosis lesions in the lower cord
- Autoimmune conditions like neuromyelitis optica
Real‑life example:
A person with poorly controlled diabetes has increasing back pain and low‑grade fevers. He dismisses it as “muscle strain.” Two weeks later, he develops numbness around the anus and difficulty walking. MRI shows an epidural abscess compressing the cauda equina. Emergency surgery and antibiotics are needed.
Prompt recognition and treatment of spinal infections can be lifesaving. Delayed care may lead to paralysis, sepsis, or chronic pain.
6. Complications From Spinal Procedures Or Anesthesia
Modern medicine uses many procedures near the spine. Most are safe, but complications can occur. These can sometimes lead to numbness in the saddle area.
Procedures that carry some risk include:
- Epidural anesthesia during childbirth or surgery
- Spinal anesthesia for operations on the legs, pelvis, or abdomen
- Lumbar puncture (spinal tap) for diagnosis
- Epidural steroid injections for back pain
- Spine surgeries, including decompression or fusion
Possible complications:
- Bleeding in the epidural space, forming a hematoma
- Infection leading to an abscess
- Direct nerve trauma, though rare
- Leakage of cerebrospinal fluid causing low‑pressure headaches and nerve stretch
Warning signs after a spinal procedure:
- New or rapidly worsening low back pain
- Leg weakness
- Numbness or tingling in the groin, perineum, or buttocks
- Loss of bladder or bowel control
- Fever or severe headache
Real‑life example:
After a routine epidural for childbirth, a patient feels fine for several hours. Later, she develops intense back pain and numbness between the legs. She also struggles to pass urine. Imaging reveals an epidural hematoma compressing the cauda equina, which is urgently removed.
If you ever notice pelvic or perineal numbness following a spinal procedure, treat it as an emergency and seek immediate care.
7. Systemic Diseases And Nerve Disorders
Most cases involve structural problems near the lower spine. However, certain systemic diseases and generalized nerve disorders can also affect sensation in the saddle region. These are less common but important.
Examples include:
- Severe diabetic neuropathy, especially if combined with spinal stenosis
- Vascular disease causing spinal cord ischemia
- Autoimmune neuropathies affecting multiple nerve roots
- Rare hereditary neuropathies
Typical features:
- Numbness and tingling starting in the feet and hands
- Gradual progression upwards over months or years
- Possible weakness, cramps, or burning pain
- Later involvement of the thighs and perineal area
Even in these conditions, new saddle numbness often triggers imaging. Doctors need to be sure no compressive lesion has developed on top of existing nerve disease.
Real‑life example:
A person with long‑standing diabetes has chronic foot numbness. Over several weeks, they notice creeping numbness in the inner thighs and perineum. Imaging reveals significant spinal canal narrowing plus diabetic nerve damage. Both issues need attention.
Treatments may include:
- Aggressive control of blood sugar and blood pressure
- Physical therapy and weight management
- Pain‑modifying medications
- Sometimes surgery if there is clear structural compression
Again, any change in perineal sensation deserves careful and prompt evaluation.
Comparison Table: Major Causes Of Saddle Area Numbness
| Cause | Onset | Key Clues | Emergency Level |
|---|---|---|---|
| Cauda equina syndrome | Hours to days | Back pain, leg weakness, urinary retention, saddle numbness | Absolute emergency, urgent surgery often needed |
| Conus medullaris syndrome | Sudden or subacute | Both leg weakness, early bladder and bowel changes | Emergency, rapid imaging and treatment |
| Spinal trauma or fractures | Immediately or within days | History of injury, back pain, new numbness and weakness | Emergency if neurological symptoms appear |
| Spinal tumors or metastases | Weeks to months | Night pain, cancer history, slowly worsening symptoms | Urgent, especially with new bladder changes |
| Spinal infections | Days to weeks | Fever, back pain, risk factors like diabetes or IV drug use | Emergency when neurological signs present |
| Procedure-related complications | Hours to days after procedure | New pain and numbness after spinal anesthesia or surgery | Emergency, needs fast assessment |
| Systemic nerve disorders | Months to years | Gradual spread from feet upward, chronic health conditions | Urgent evaluation, but often less sudden |
Recognizing Warning Signs: When To Go To The ER
Regardless of the underlying reason, certain symptoms mean you should not wait. Seek immediate emergency care if you notice:
- New numbness in the perineum, anus, or inner thighs
- Sudden loss of urinary control or inability to urinate
- New bowel incontinence or severe constipation with numbness
- Weakness in both legs, especially if it worsens quickly
- Severe low back pain with any of the above signs
- Recent spinal procedure followed by new pelvic numbness
If you feel unsure, it is safer to be seen and checked. Emergency teams can assess you with a focused exam and imaging. The risk of doing nothing is far greater than the risk of seeking help.
How Doctors Decide On Treatment
Treatment depends completely on the cause. However, the principles are similar:
- Relieve pressure on the spinal cord or nerves if present.
- Treat infection, inflammation, or tumors aggressively.
- Support bladder, bowel, and sexual function as much as possible.
- Start rehabilitation early to maximize recovery.
Common treatments:
- Emergency surgery for cauda equina syndrome, trauma, or abscesses
- Steroids in selected cases to reduce swelling around the cord
- Antibiotics or antifungals for infections
- Chemotherapy, radiation, or targeted therapy for tumors
- Physical and occupational therapy to regain strength and function
- Bladder training, pelvic floor therapy, and continence supports
Recovery can be slow. Some nerve damage may be permanent, especially if compression lasted too long. Early action offers the best chance for improvement.
Living With Residual Symptoms
Unfortunately, some people continue to have numbness or bladder and bowel issues even after treatment. This can affect self‑esteem, relationships, and daily life.
Helpful strategies:
- Work with a neurologist and rehabilitation specialist
- See a pelvic floor therapist for continence and sexual function tips
- Consider counseling or a support group to manage emotional stress
- Use protective pads or clothing to feel more secure in public
- Schedule regular check‑ins with your care team
Tools like intermittent self‑catheterization, bowel programs, and adaptive equipment can restore independence. Many people return to work and fulfilling relationships with the right support.
FAQs About Saddle Area Numbness
Is any numbness in the groin an emergency?
Not every tingling feeling is an emergency. However, new, clearly reduced sensation in the perineum or anus, especially with bladder or bowel changes, should be treated as an emergency until proven otherwise.
Can back pain alone cause this symptom?
Simple muscle strain rarely causes numbness in the saddle region. When this pattern appears, doctors look beyond ordinary back pain for deeper nerve or spinal cord problems.
How do doctors confirm the diagnosis?
They combine your history, a focused neurological exam, and imaging of the spine. The most important tool is usually an MRI of the lumbar and sacral regions.
Can the numbness go away on its own?
Sometimes mild numbness improves if the underlying cause is treated quickly. If nerve compression continues, numbness may become permanent. That is why early evaluation is crucial.
Is it always caused by a herniated disc?
No. A large disc herniation is a common cause, but tumors, infections, trauma, and complications from procedures can also lead to the same symptom pattern.
What should I tell the doctor if this happens?
Describe exactly where you feel numb, when it started, and any changes in bladder, bowel, or sexual function. Mention recent injuries, infections, procedures, or known cancers. This information guides rapid decisions about imaging and treatment.
Conclusion: Listen To What Your Nerves Are Telling You
Numbness or strange sensations in the groin, inner thighs, or buttocks are easy to feel embarrassed about. Many people delay care because they hope it will fade. Yet this pattern, often described clinically as saddle anesthesia, is one of the body’s most serious warning signs.
Understanding what is happening can help you move from fear to action. You have learned the major saddle anesthesia causes, the key symptoms to watch, and how doctors test for them. You also know which red flags demand immediate emergency attention.
If you ever notice these changes, especially with bladder or bowel problems, treat them as urgent. Contact emergency services or go directly to the nearest hospital. Early diagnosis and treatment offer the best chance to protect your mobility, independence, and quality of life.
If you live with chronic back issues or nerve problems, consider discussing this specific symptom pattern with your healthcare provider at your next visit. You can also explore related topics, like understanding lumbar disc herniation or peripheral neuropathy, to deepen your knowledge.
Your spine and nerves do important work every second. When they send a warning, it is worth listening—and acting—right away.